Learn how this revolutionary initiative can improve healthcare quality and access for you and your family.
The federal government is working to implement a single, integrated electronic health record system for agencies like the VA to improve care coordination and delivery. This effort aims to simplify healthcare through upgraded technology and enhanced data sharing across providers.
If you or a loved one has served our country, you know that navigating healthcare through the VA can be complicated. With so many doctors and facilities involved, important health information doesn’t always make it where it needs to go. But what if we told you there is an exciting new initiative to fix this problem?
The federal government is working to modernize electronic health records for veterans and other federal beneficiaries. This effort aims to improve care coordination and delivery through an integrated, easy-to-use system.

The Federal Electronic Health Record Modernization (FEHRM) program is an initiative to implement a single, common electronic health record system across federal agencies. The goal is to simplify and streamline healthcare for veterans, service members, and other federal health beneficiaries.
Right now, health records are fragmented across the Department of Veterans Affairs (VA), Department of Defense (DOD), and other agencies. This lack of coordination leads to repeat testing, missed diagnoses, medication errors, and delays in treatment. Not ideal!
Under the FEHRM program, agencies like the VA, DOD, U.S. Coast Guard, and National Oceanic and Atmospheric Administration will transition to the same centralized network. This means your health history, test results, treatments, and more will be accessible to any of your care providers, no matter where you’re seen. Cool, right?
The modernized electronic health record system has some amazing features in the works to improve your care experience:
With the new system, the VA, DOD, and community health partners can seamlessly share vital health data. This prevents information gaps when transitioning between providers.
Your full medical history will be available in one place for a more complete picture of your health. No more carrying stacks of printed records between doctors!
Your healthcare teams will have access to the latest tools to analyze health trends, identify risks, and provide more personalized care tailored to you.
The system will enable proactive monitoring and interventions when health concerns arise. This supports better safety and outcomes.
This initiative is already well underway with over 194,000 users onboard across participating agencies:
Of course, with any huge IT overhaul, there have been some bumps in the road:
Despite these temporary setbacks, the VA is working diligently to implement the new technology successfully. The benefits to veteran care are abundantly clear as kinks are worked out.
For our veterans, this new technology has immense potential to improve care quality and simplify navigating the VA healthcare system:
With interconnected records, you won’t have to repeat health information or tests every time you see a new VA provider. Appointments and procedures can happen more quickly.
Your medical history can be analyzed to predict health risks and ensure you get appropriate screenings and preventive care. This is especially helpful for issues related to your service.
By tracking your full health profile, risks like PTSD, depression, suicide ideation can be identified sooner and addressed through proactive interventions.
Integrated prescription drug monitoring will help minimize opioid abuse and “doctor shopping” for controlled medications.

The FEHRM program isn’t happening in isolation. It’s part of a larger move towards data integration and efficiency across both federal and private healthcare:
The FEHRM serves as a foundation for the future of healthcare technology innovation. As successes are proven, more advanced capabilities like telehealth, clinical decision support, and predictive analytics will continue evolving.
At the end of the day, this about improving care for our nation’s veterans, service members, and federal health beneficiaries. With continued progress, the modernized EHR system will:
While the program continues rolling out, don’t hesitate to share any feedback with your VA providers so adjustments can be made. We’re all in this together to ensure the promise of technology aligns with the needs of patients!
Discover how evolving regulations drove innovation in electronic medical records and propelled healthcare's digital transition.
HIPAA began influencing EHR development in the 1990s as digital records grew, though major effects came after the HITECH Act expanded privacy rules in 2009.

The Health Insurance Portability and Accountability Act (HIPAA) was signed into law in 1996. This landmark legislation aimed to reform the healthcare industry by improving insurance coverage portability when changing jobs and reducing fraud.
Importantly, HIPAA also mandated new standards for the privacy and security of individuals’ identifiable health data, known as protected health information (PHI). This included provisions to:
The original HIPAA privacy regulations were intentionally broad, establishing general definitions and principles for PHI use. This preceded the widespread adoption of EHR systems.
Back then, paper medical records were still commonplace. So initially, HIPAA did not substantially affect medical record software or technology.
In the 1960s and 1970s, academic medical institutions started developing their own localized EHR systems. But it wasn’t until the 1980s that momentum built for industry-wide EHR standards.
Leaders recognized the need for common guidelines if digital records were to fulfill their potential. Interoperable systems that could “talk” to each other were essential for productive information exchange.
This led to the formation of standards development organizations (SDOs) focused entirely on EHRs. One of the most prominent was Health Level Seven International (HL7), established in 1987.
HL7 has played a key role in enabling system integration. Their interoperability standards allow the components of EHR systems to share and understand data. This makes it possible for patient information to flow securely between clinics, labs, pharmacies, insurers, and other entities.
As EHR adoption expanded in the 1990s, HIPAA’s general principles gained more specific relevance to electronic systems. For example, standards were needed for user authentication, audit trails, and other security controls required by HIPAA.
While HIPAA laid the data privacy and security groundwork, the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 really accelerated EHR implementation.
It did so by:
Essentially, the HITECH Act both strengthened HIPAA and motivated EHR adoption by complicating compliance for late adopters. By tying privacy enforcement and system reimbursements together, it propelled healthcare rapidly into the digital age.

Today, healthcare providers using EHR platforms must maintain compliance with HIPAA regulations. This influences software design and functionality in a few key ways:
Essentially, HIPAA sets ground rules for EHR security capabilities and practices. From access management to disaster recovery provisions, these standards define the regulatory guardrails EHR systems operate within.
EHR developers must constantly monitor HIPAA requirements and adapt platforms accordingly. They also support customers with compliance by providing necessary privacy and security features.
For healthcare providers, this means choosing EHR solutions carefully to avoid gaps that could lead to breach risks and penalties. Partnering with vendors up-to-date on the nuances of HIPAA ensures systems can be trusted to safeguard patient data.
In summary, the histories of HIPAA standards and EHR technology adoption are very much intertwined. The increasing prevalence of digital records created a need for more stringent, specific privacy and security regulations. And in turn, those evolving regulations drove further EHR innovation.
This interplay continues today, as technology and regulatory guidance evolve in lockstep to balance data access, integrity, and protection for optimal healthcare delivery.
| Year | Key Development |
| 1996 | HIPAA enacted with initial privacy and security standards |
| 2009 | HITECH Act expanded HIPAA rules and incentivized EHR adoption |
| Present | Ongoing refinements to standards and platforms |
The passage of HIPAA and especially the HITECH Act were pivotal moments that accelerated paper-to-digital health data transitions through incentives and enforcement. But work is ongoing to refine standards and maximize benefits from EHR systems.
For providers, staying up-to-date on the latest HIPAA guidance is essential to fully leverage technology while managing compliance risks. And for EHR vendors and developers, anticipating regulatory shifts allows building platforms ready to meet the demands of contemporary healthcare.
Understanding this historical give-and-take dispels any notion of HIPAA standards as static or detached from real-world practice. They are an integral force shaping the possibilities and direction of EHR systems and digital health overall.
Running an IV therapy practice comes with unique workflow and documentation demands. Choosing the right electronic medical record (EMR) system is critical for efficiently managing your practice while delivering top-notch care.
But with so many EMR platforms out there, how do you select the perfect one for your IV therapy clinic?
EMR software designed specifically for IV therapy clinics offers tailored tools and features to align with your particular documentation, ordering, and care coordination needs.
General EMR systems without dedicated IV therapy capabilities often lack key functionality like:
Without an EMR designed for IV therapy workflows, clinics sacrifice efficiency, accuracy, regulatory compliance, and more.
To manage IV infusion workflows smoothly, an EMR must have the right clinical tools tailored to this specialty while supporting robust practice management.
Here are some of the most essential features to look for:
| Tool Feature | Description |
| Pre-built IV therapy note templates | Documentation forms with sections for infusion details, IV site, adverse reactions, and other relevant clinical data. |
| Catalog of IV fluid and medication options | For quickly selecting the correct infusions and dosages during order entry. |
| E-prescribing and pharmacy integrations | To electronically prescribe fluids, infusion drugs, pumps, tubing, etc. |
| Infusion schedule tracking | Displays upcoming and past infusions for coordination and medication refills. |
| IV catheter/site documentation | Logs details like site location, date inserted, required rotation, and more. |
| Inventory management | Tracks supplies and IV medication stock levels. |
| Tool Feature | Description |
| Scheduling and appointment reminders | Manages infusion appointments and sends automated reminders. |
| Billing and claims management | Handles insurance claims related to IV therapy services. |
| Analytics reporting | Tracks IV clinic KPIs like infusion volumes, common medications, revenue, etc. |
| Patient portal | Allows self-scheduling, bill pay, medication refill requests, and record access. |
| Referral management | Tracks and communicates with referring providers. |
EMR costs differ widely based on the vendor, features, and practice size. Here are rough estimates for IV therapy practices to budget accordingly:
To control costs, look for systems like cloud-based platforms with minimal upfront license fees and predictable subscription pricing. Scalable subscriptions allow managing costs as your IV practice grows.

What sets Calysta EMR apart is its dedication to IV therapy providers like you. Say goodbye to generic EMR systems that fail to meet your unique requirements. With Calysta EMR, you'll have access to a suite of specialized features tailored to your IV therapy practice.
With Calysta EMR's online patient booking feature, your patients can conveniently schedule their appointments from the comfort of their homes. And with automated appointment reminders and synchronized staff calendars, you'll never miss a beat – ensuring efficient scheduling and minimizing overlaps.
Keeping track of your IV supplies and medications can be a daunting task, but Calysta EMR has your back. With real-time inventory tracking, automated reordering, and stock level alerts, you can say goodbye to the nightmare of running out of crucial supplies.
Administrative tasks can be a time-suck, but not with Calysta EMR's task automation capabilities. Customizable workflow automation means your staff can streamline repetitive processes, boosting productivity and freeing up valuable time for patient care.
In today's world, contactless transactions are a must, and Calysta EMR delivers with its integrated payment processing feature. Your patients can complete secure and touchless payments with ease, ensuring a hassle-free experience that keeps everyone safe and satisfied.
As a cloud-based platform, Calysta EMR is accessible from anywhere, anytime, ensuring you and your team can access crucial patient data and documentation on the go. And with automatic data backups and updates, you can rest assured that your information is always safe and up-to-date.
Calysta EMR takes data security seriously, operating on HIPAA-compliant servers to safeguard your patients' sensitive information. No more worrying about breaches or compromised data – with Calysta EMR, you can focus on providing quality care with peace of mind.
If you're already using a practice management system, Calysta EMR seamlessly integrates with it, ensuring a centralized hub for all your patient data and financial information.
While paper charts may seem simpler for a smaller clinic, an EMR still offers major advantages even if you only have 1-2 providers. Benefits like legible documentation, simplified record access, reduced duplication, and more coordinated care make EMR adoption worthwhile regardless of practice size. Cloud-based systems have made EMRs affordable for practices of all sizes.
Quality EMR vendors provide extensive training resources, including videos, manuals, webinars, and onsite support to guide your team's adoption. Look for vendors that provide advisory services customizing the system to your unique workflows.
Ask vendors about their data migration process – it should be structured with validation testing. Disruption can be minimized by archiving old system data but accessing it read-only when needed. With adequate preparation and training, switching EMR systems can be a smooth experience.
At minimum, IV therapy EMR vendors should provide encrypted data transmission and storage, role-based access controls, detailed audit logs, remote data wiping for lost/stolen devices, scheduled system backups, and robust disaster recovery capabilities. Advanced options like two-factor authentication and single sign-on further heighten security.
Getting clinician buy-in requires demonstrating how an EMR with IV therapy-specific features improves workflows and quality of care. Showcasing time savings from documentation templates, reduced transcription errors, better coordination through infusion tracking, and safer e-prescribing can resonate with providers. Offering robust training and on-demand support can ease the transition as well. With a smooth implementation focused on enhancing patient care, EMR adoption can succeed.
Implementing an electronic medical record system fine-tuned for IV infusion workflows is a foundational yet strategic move for IV therapy practices looking to scale up efficiency and care quality.
With attention to must-have features for documentation, practice management, value-added vendor services, and costs, IV clinics can thrive with the right technology partner. The improved coordination, accuracy, regulatory compliance, and streamlined administrative workflows empower IV infusion practices to deliver their life-enhancing services at the highest levels.
Improving electronic health records (EHRs) involves enhancing their accuracy, accessibility, and interoperability. This can be achieved by implementing user-friendly interfaces, integrating AI-powered tools for data analysis, and ensuring seamless data exchange between different healthcare systems.
Electronic health records (EHRs) have become an indispensable part of modern medical practices. However, simply implementing an EHR system is not enough. To fully realize the benefits of EHRs, you need to optimize their use for your unique practice needs.
In this comprehensive guide, we provide key insights and actionable steps on how to improve your EHR system, boost efficiency, enhance patient care, and take your practice to the next level.

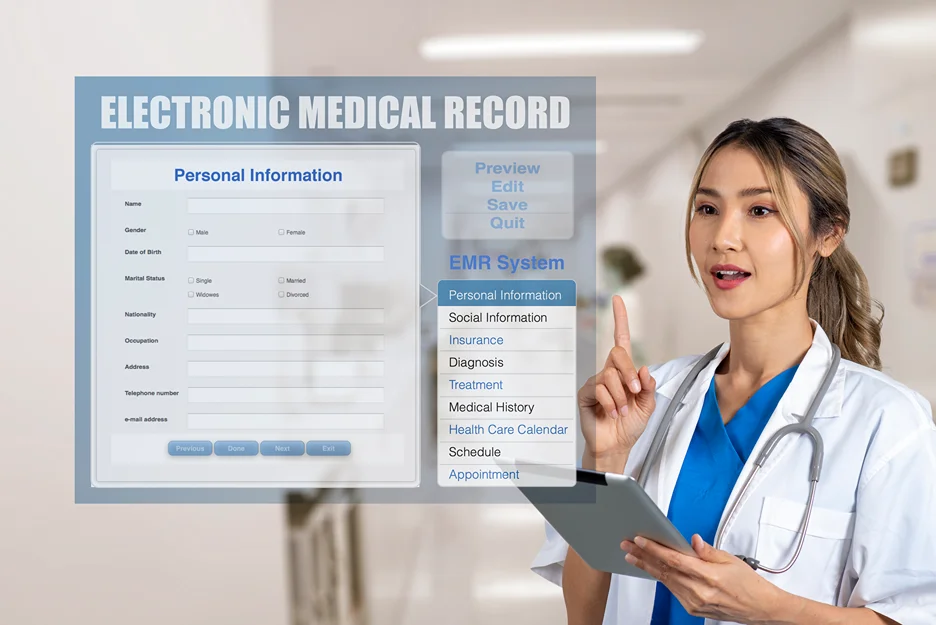
An EHR is an electronic version of a patient's medical history that is maintained digitally by healthcare providers over time. This includes information like patient demographics, medical and surgical histories, medications, vital signs, immunizations, laboratory data, and radiology reports. The EHR allows a patient's health information to be accessed and shared securely across different healthcare settings.
The overarching goals of EHR systems are to:
See how Calysta EMR can streamline your practice's patient care and workflow - book a demo today!
Implementing an electronic health record (EHR) system presents countless opportunities as well as challenges for healthcare organizations. While EHRs contain troves of valuable patient data and enable enhanced care coordination, realizing their full potential requires thoughtful design and continuous optimization.
For many clinicians, learning to use an EHR system can be frustrating and disruptive to workflow. The good news is that improving EHR usability is possible with a few key strategies:
| Strategy | Description |
| Streamline Data Entry with Templates and Macros | Leverage templates for documentation and macros for commonly repeated tasks. This reduces repetitive typing and saves time during patient visits. |
| Implement Intuitive Interfaces | Well-designed interfaces with logical menu layouts, minimal clicks, and search functionality can simplify EHR navigation. Evaluate your system to identify areas for improvement. |
| Provide Ongoing EHR Training | Conduct periodic training refreshers on optimal EHR use. This helps users stay up-to-date as new features are added. |
When thoughtfully implemented, these steps help standardize EHR use across your practice for a more intuitive and efficient clinician experience.
Fragmented patient information across different healthcare systems is a major roadblock. Lack of interoperability can negatively impact care coordination and patient outcomes. Here are some tips to improve data exchange:
EHRs should complement and enhance, not hinder, patient care workflows. Consider these workflow optimization strategies:
| Strategy | Description |
| Automate Manual Processes | Identify repetitive manual tasks that can be automated through macros, alerts, and workflows. This reduces administrative burden on clinicians. |
| Reorganize EHR Displays | Evaluate if your EHR displays information in a logical manner consistent with your clinical workflow. Rearrange menus and tabs accordingly. |
| Create Specialty-Specific Templates | Design documentation templates around common diagnoses and visits specific to your practice specialty. This supports efficient clinical decision-making. |
By aligning EHR configuration more closely with real-world care workflows, practitioners can provide care more intuitively and efficiently.
Optimize your clinical workflows effortlessly with Calysta EMR, automating manual processes and tailoring templates to your specialty for efficient decision-making
Incomplete or inaccurate data in EHRs can undermine care quality and hinder population health management. Some best practices include:
With robust protocols and validation measures, practices can tap into EHRs as a source of trustworthy clinical data and advanced analytics.
Electronic health records (EHRs) contain highly sensitive and private patient information, making them a prime target for cyberattacks and data breaches. Medical practices must take proactive measures to safeguard EHR systems and patient data from unauthorized access, including multi-layered defense strategies like:
Implement role-based access controls to restrict EHR functionality and data access. Provide access on a need-to-know basis using the principle of least privilege. Regularly review user permissions and disable inactive accounts. Using strong passphrases instead of passwords provides another layer of protection.
Leverage data encryption technologies to secure patient information in transit and at rest. Encrypt data whether it is moving over a network, sitting on servers or devices, or recorded on removable media. This helps safeguard data privacy if devices are lost or stolen.
Install comprehensive security software such as antivirus, anti-malware, firewalls, intrusion detection/prevention systems (IDS/IPS), and data loss prevention (DLP) solutions. These provide layered cybersecurity monitoring and protection against threats like malware, ransomware, phishing attacks, and improper data exfiltration.
Conduct routine risk assessments to identify and address potential vulnerabilities in your EHR environment before they can be exploited. Assessments should cover the EHR application, network, endpoints, access controls, physical security, policies and procedures, training, and third-party connections.
Implement regular cybersecurity and privacy awareness training to keep employees up-to-date on the latest threats and organizational policies. Alert fatigued staff to watch for fraudulent emails, texts or phone calls asking for personal information.
Develop a formal incident response plan for security breaches, including roles and responsibilities, communications protocols, and integration with law enforcement if necessary. Being prepared can help limit damages and expedite recovery.
By taking a proactive approach to EHR security through continuous risk analysis, training, system hardening and data protection, healthcare providers can better safeguard these critical information systems and the sensitive data they contain.
Protect your patients' sensitive data with Calysta EMR's robust security measures and proactive risk assessments for peace of mind

EHR systems were not originally designed to harness the power of artificial intelligence (AI) and wearable devices. By integrating these emerging technologies, healthcare organizations can unlock new potentials to optimize EHRs, improve clinical workflows, and enable more proactive and personalized care models.
Look to emerging technologies to unlock new possibilities for EHR optimization:
Incorporate natural language processing, deep learning, and predictive analytics algorithms that can analyze patient data from lab results, medical history, and other sources in the EHR. The algorithms provide real-time diagnostic and treatment recommendations to clinicians at the point of care to augment their decision-making. This AI support allows doctors to provide more evidenced-based, personalized care.
Allow patients to sync data from consumer wearable devices like Fitbits, Apple Watches, glucose monitors and more to their personal health records. This provides doctors with more comprehensive, real-time data on the patient's lifestyle, biometrics, and health indicators outside the clinic. The additional holistic health data helps inform better care.
Implement accurate voice recognition and transcription to allow doctors to narrate clinical notes, reports, and other documentation, reducing typing time. This saves physicians time on administrative work and improves documentation detail and quality as they can speak freely. Ensure proper AI training on medical terminology for reliable documentation.
Provide telehealth platforms for remote video visits, allowing patients to conveniently conduct appointments with their doctors online. Integrate virtual assistants like chatbots to automate administrative tasks for doctors and patients like appointment booking, prescription refills, medical bill payments and more. This improves access and efficiency.
Expand patient portals with features like customized health education resources, medication management tools, and secure messaging with physicians. Integrate wearable data into portals to give patients greater ownership over their health data. Improved portals and wearables boost patient engagement, satisfaction, medication adherence, and outcomes.
By embracing cutting-edge innovations, forward-thinking practices can chart an advanced path for the future of EHR systems.
At Calysta EMR, our mission is to create intuitive software that simplifies EMR use for aesthetic medicine practices. Our specialty-specific EMR system and seamless workflows empower you to focus on delivering excellent aesthetic care while optimizing documentation, billing, scheduling, and more.
Book a demo today to learn how Calysta can help your practice succeed by moving beyond a basic EHR to an intelligent informatics platform. Our knowledgeable team is ready to answer your questions and get you on the path to elevating your EHR capabilities.
The need for electronic health records (EHRs) was catalyzed by the desire to improve healthcare quality and safety. This change was also driven by the potential for EHRs to enhance efficiency and coordination in healthcare delivery.
Paper-based medical records have been the norm in healthcare for over a century. However, the limitations of handwritten patient charts have become increasingly apparent in our modern, data-driven world.
Electronic health records (EHRs) promise improved care coordination, enhanced patient engagement, and streamlined administrative tasks. But what factors drove healthcare providers to make the switch from paper to pixels in the first place?
In this article, we’ll explore the catalysts behind the rise of EHRs and why they’ve become a necessity for forward-thinking practices. We’ll also look at the key benefits EHRs offer patients and providers alike. Read on to learn how digitizing patient records can transform your practice!
Take your practice to the next level with Calysta EMR and experience seamless access to comprehensive patient information and streamlined administrative tasks

Electronic health records (EHRs) aim to improve healthcare delivery and patient outcomes through the digitization of health information. EHRs are comprehensive records that provide a complete view of a patient's medical history, including demographics, progress notes, medications, immunizations, radiology reports, and more. The EHR is designed to be a real-time, patient-centered record that makes information available instantly and securely to authorized users.
Some key components and capabilities of an EHR system include:
The main catalyst for EHRs was a two-pronged approach:
Paper-based records made it difficult for providers, especially specialists, to access a patient's full medical history. This could lead to delays in diagnosis, treatment, and potential errors due to incomplete information. EHRs aimed to solve this by creating a centralized, accessible electronic record.
Paper records are not only cumbersome but also expensive to manage and store. Additionally, administrative tasks like billing and coding were time-consuming. EHRs promised to streamline these processes, making healthcare administration more efficient and potentially reducing overall costs.
While both aspects were important, the initial push for EHRs likely came from the desire to enhance patient care by ensuring complete and readily available medical information.
Electronic Health Records aren't necessarily mandatory, but they've become increasingly necessary in modern healthcare due to several key advantages over traditional paper charts. Here's why EHRs are crucial:
While EHRs enhance care delivery, they also create a more streamlined administrative workflow. Automating manual tasks like appointment scheduling and billing coding frees up staff to focus on patient support. The data in EHRs can even be used to analyze practice trends over time.
Elevate patient care and efficiency in your practice with Calysta EMR's integrated solutions for improved coordination, safety, and decision-making
Electronic health records provide transparent access to their complete medical histories. With EHRs, patients can view test results, treatment plans, and clinical notes online through patient portals. This transparency enables patients to take a more active role in their healthcare and make informed decisions.
EHRs also allow patients to connect external health data from wearable devices and health apps to their records. Integrating these additional data sources gives patients a comprehensive view of their health and helps them collaborate more effectively with providers.
An important benefit of EHRs is the ability to track who accesses records and when through audit trails. This increases accountability and gives patients greater control over their personal health information. Overall, EHRs aim to put health data in patients' hands, engage them in their care, and build more collaborative patient-provider relationships.

Regulatory requirements have been a major driving force behind the widespread adoption and meaningful use of electronic health records (EHRs). Regulations have accelerated EHR implementation in several key ways:
Government agencies have defined technical standards and certification criteria to ensure proper data exchange, privacy protection, and systems integration across diverse EHR platforms. This has reduced fragmentation and enabled more coordinated care.
Programs like the HITECH Act in the US have provided financial incentives for providers to implement EHRs and utilize them in impactful ways that improve quality, safety, and efficiency. Meeting meaningful use criteria has been required to receive incentives.
Regulations have mandated specific EHR capabilities and data capture to aid clinical decision support, such as flags for duplicate tests, drug interaction alerts, and reminders for preventive care. This has reduced errors and improved adherence to evidence-based guidelines.
Standardized data formats and transmission protocols have allowed EHRs to seamlessly submit reportable clinical data to public health agencies, facilitating disease surveillance and response.
Policy frameworks have been established for responsibly leveraging EHR data for research while maintaining patient privacy, catalyzing data-driven health improvements through the analysis of real-world evidence.
While regional contexts vary, regulations have fundamentally shaped EHR systems into more robust tools for enhancing individual and population health outcomes. Policy initiatives have progressed EHRs beyond just digital record-keeping to become integral platforms for driving healthcare value.
Stay compliant and maximize incentives with Calysta EMR's tailored solutions that meet regulatory standards and enhance clinical decision-making
EHRs can reduce errors by providing clinical decision support, like drug interaction alerts. They also eliminate issues with illegible handwriting.
On average, it takes about 6-12 months to fully transition a practice from paper to electronic records, including planning, system selection, training, and optimization.
Yes, patients have the right under HIPAA to request changes to their records if they believe information is incorrect or incomplete. The provider can accept or deny the request.
Yes, many EHR systems can interface with medical devices to auto-populate vital signs, test results, and other clinical data, eliminating manual entry.
Yes, EHRs allow concurrent editing by multiple users. The system tracks all changes, maintaining a detailed audit trail.
The digitization of health records is transforming modern medicine by removing information silos, engaging patients, and driving evidence-based care. EHRs began as a solution to the fragmented nature of paper-based records but have since evolved into sophisticated platforms with countless applications for improving health outcomes.
At Calysta EMR, we understand the catalysts behind this digital health revolution. Our intuitive EMR system was designed by Dr. Hardik Soni to meet the specific needs of modern practices. Calysta EMR makes it simple to access complete patient information, coordinate referrals, engage patients through portals, and automate administrative tasks, and we do this at a fraction of the cost of competing solutions.
To learn more about bringing the advantages of EHRs to your practice, contact our team today. It's time to take the leap into digital health and unlock the benefits of EHRs for your patients and providers alike. Experience the Calysta difference!
Electronic medical records (EMRs) and electronic health records (EHRs) bring undeniable advantages to healthcare, but proactive security measures, government regulation, and multi-stakeholder collaboration are essential to safeguard sensitive patient data and preserve trust in the digital healthcare system.
Electronic medical records (EMRs) and electronic health records (EHRs) have become integral parts of the healthcare system. By digitizing patient information that was previously stored on paper, EMRs and EHRs allow for more efficient storage, retrieval and sharing of health data. However, the benefits provided by electronic records come with inherent security risks that cannot be ignored.

EMRs and EHRs contain a wealth of sensitive personal health information (PHI) that makes them prime targets for cyberattacks and data breaches. Some of the main vulnerabilities that put EMR/EHR security at risk include:
EMR/EHR systems can be compromised by outside hacking or malicious insiders misusing their access privileges. Tactics like phishing or exploiting weak passwords allow unauthorized parties to gain access to medical records. Patient PHI may then be stolen and sold or used for identity fraud.
Without proper safeguards, EMR/EHR data can be altered intentionally or accidentally in ways that compromise patient safety. Errors in data entry, malware infections, and ransomware attacks can all lead to corruption or loss of medical records. Inaccurate or missing health data prevents proper patient care.
Many healthcare organizations rely on legacy EMR/EHR systems that lack the latest security features and patches. Technical vulnerabilities in outdated platforms increase the risk of cyberattacks and system failures that cause health data breaches or downtime.
EMR/EHR data that is transmitted or stored without encryption is vulnerable to interception by malicious actors. Improper configuration of cloud-based storage can also expose PHI. Lack of data encryption and auditing makes it challenging to track breaches.
Security breaches involving EMRs and EHRs can have far-reaching consequences for patients, healthcare providers, and the trust placed in the healthcare system. Here are some of the most significant impacts:
The theft of Protected Health Information (PHI) allows perpetrators to use it to file fraudulent insurance claims, obtain prescriptions and services under a patient's name, or even commit broader financial identity theft crimes.
Violations of patients' privacy caused by unauthorized access or leaks can expose highly personal medical information. This exposure can lead to discrimination, embarrassment, and reputational harm for the individuals affected.
Ransomware attacks or data breaches that lock healthcare providers out of their systems disrupt regular care. The inability to access medical records during emergencies can also significantly delay diagnosis and treatment, potentially leading to adverse health outcomes.
When patients learn their sensitive health information has been exposed, it erodes their trust in providers to protect their data. Patients may become reluctant to share vital information or avoid seeking necessary care as a result.
The government plays a multi-faceted role in safeguarding the security of EMR/EHR systems. Its influence extends from the foundational frameworks provided by HIPAA and the HITECH Act to current and evolving initiatives aimed at balancing health data security with innovation and interoperability. Here are the important aspects of government’s influence:
These acts are the cornerstone of patient privacy and health data security regulations. HIPAA's Security and Privacy Rules outline technical, physical, and administrative safeguards required of covered entities to protect ePHI. HITECH expanded HIPAA's scope, introduced stricter enforcement, and spurred the adoption of certified EHR technology. Recent years have seen an increase in enforcement actions, highlighting the government's commitment to holding covered entities accountable for security lapses.
Cybersecurity threats facing the healthcare sector are constantly evolving. The government recognizes the need for the legal framework to adapt accordingly. This might include:
A key government focus is on facilitating the seamless and secure exchange of health information to improve care coordination and patient outcomes. Initiatives like these demonstrate this focus:
The government's role in EMR/EHR data security extends beyond laws and enforcement. It involves fostering collaboration between various stakeholders to address security challenges, including:

Healthcare organizations play a critical role in protecting the sensitive data within EMR/EHR systems by taking proactive measures including:
Enforce strict password policies, implement role-based access levels, use multi-factor authentication, and promptly revoke former employee credentials. Limit system access only to necessary users.
Conduct regular EMR/EHR risk analyses and vulnerability scanning. Monitor systems for suspicious activity to identify threats early. Update controls to address new risks.
Train staff on secure data handling through HIPAA compliance programs. Test defenses with simulated phishing attacks. Ensure personnel at all levels understand EMR/EHR security policies.
Have detailed procedures in place to contain, investigate, and remediate breaches. Educate employees on responding appropriately to ransomware, hacking attempts, unauthorized access, and similar incidents.
EMRs and EHRs provide invaluable benefits for improving quality of care and patient outcomes. However, as sensitive data repositories, they also attract cybercriminals seeking financial gain or disruption.
Through vigilant security defenses, compliance with regulations, employee training, and collaboration between government, healthcare organizations, and health IT vendors, the security risks inherent in EMR/EHR systems can be mitigated.
At the same time, we must find the right balance to preserve the systems’ advantages for efficiency, cost-effectiveness, and ultimately better medical care. Patients also have a role in exercising their rights over personal health data security and holding the healthcare system accountable.
EHRs improve communication in healthcare by providing a centralized digital platform that facilitates seamless information sharing between providers, patients, and healthcare settings.
Smooth and seamless communication is the lifeblood of effective healthcare. From coordinating care between different providers to keeping patients informed about their health, clear and efficient sharing of information is essential. This is where electronic health records (EHRs) can make a major impact.
Implementing EHR systems has the potential to greatly enhance communication for healthcare organizations across the board. But realizing these benefits depends on choosing the right system, proper training, and putting patients at the center of the process.
First, it’s helpful to understand exactly what we mean by “EHR.” EHR stands for electronic health record and refers to the comprehensive digital record of a patient’s health data across multiple care settings. This includes medical history, diagnoses, medications, immunizations, test results, and more.
EHRs differ from EMRs (electronic medical records) in their scope. EMRs are digital records specific to one healthcare organization. So a single doctor’s office may have its EMR system for medical data related only to that practice. EHRs pull together the full health record from multiple sources into one integrated system.
Both EMRs and EHRs offer tools to enhance clinical workflow and communication compared to paper records. But EHRs provide the complete patient story, facilitating seamless information sharing between various providers.

One of the biggest communication challenges in healthcare is coordinating care across a patient’s whole care team. This team may include primary care doctors, specialists, nurses, physical therapists, social workers, and other providers. Crucial health details often fell through the cracks with paper records and faxed documents. EHRs offer several ways to streamline provider-to-provider communication:
All providers authorized to view a patient’s EHR can immediately see up-to-date information entered by other team members. Lab results, specialist reports, and new medication orders populate the record in real-time. This mitigates the game of “phone tag” between offices chasing down needed patient info.
EHR systems include built-in messaging functionality as a quick way to communicate with other providers. Messages become part of the patient record and avoid the security risks of consumer email services.
The EHR referral management tools allow providers to electronically send and track referrals or specialty consultation requests. This facilitates getting patients needed appointments faster and specialists can easily view the patient’s full record.
Seeing the full medication list and prescription history from within the EHR allows providers to coordinate prescriptions and reduce risks of adverse drug interactions.
This real-time, shared access is especially critical for transitions between care settings. For example, when a patient is discharged from the hospital, their primary care doctor immediately sees the hospitalization details, discharge instructions, new prescriptions, and follow up needs. This continuity of information facilities coordinated care.
In addition to improving inter-provider communication, EHRs also enhance how healthcare teams connect directly with patients:
Portals allow patients 24/7 access to their personal health records. They can view test results, upcoming appointments, immunization records, and more. Many portals also allow patients to directly message their providers.
Patients don’t need to wait for a provider visit to view their information or send a message. Providers can also communicate with patients outside of visits (e.g. sending reminders about needed follow-up tests).
Many EHR portals enable online appointment scheduling. Patients can book at their convenience without waiting on hold during clinic hours.
Portals may offer integrated patient education resources. Providers can push educational materials related to diagnoses, medications, and treatment plans directly to the patient’s portal.
This transparency supports patients taking an active role in their care and strengthens the patient-provider relationship.
Fragmentation between healthcare organizations has long hindered coordinated, team-based care. Traditionally, sending records via fax or CD-ROM when patients transitioned between settings often led to gaps in care. However, modern advancements have significantly improved communication possibilities.
EHRs can enhance cross-setting communication, with interoperability (the ability to exchange computable data) being crucial. Standards like Fast Healthcare Interoperability Resources (FHIR) are advancing data-sharing capabilities, and other modern tools like Health Information Exchanges (HIEs) and secure messaging facilitate information exchange.
Here are some examples of how EHRs streamline communication:
When patients move between care settings (like hospital to rehab facility to home), EHR data transfer prevents information gaps. For example, discharge summaries from the hospital populate right into the primary care EHR to facilitate smooth follow-up.
ER doctors can access the patient's full medical history even if they're unconscious or unable to communicate, allowing for better diagnosis and treatment in emergencies.
EHRs can facilitate real-time reporting of infectious diseases and tracking of disease outbreaks when connected to public health agencies.
Overall, this interoperability enables true care team collaboration, leading to more coordinated treatment plans and better health outcomes.

Numerous studies demonstrate the benefits of EHRs on healthcare communication and related outcomes:
The evidence strongly supports EHRs' potential to connect healthcare teams and patients when thoughtfully implemented.
While EHR adoption continues to climb, implementation challenges can hamper realizing the full communication potential. Here are some best practices to maximize EHR communication capabilities:
Effective change management ensures your organization gets the most from the EHR communication tools.
While EHRs offer major communication advances, being aware of potential challenges and proactively addressing them is important:
| Challenge | Potential Limitations | Mitigation Strategies |
| Privacy Concerns | Sensitive health information in EHRs raises privacy risks if not carefully managed. | Implement strong access controls and granular permissions to protect patient data within the EHR. Staff should undergo thorough training on HIPAA compliance and ethical data sharing practices. Additionally, patients should be educated about their privacy rights and how their data is utilized. |
| Information Overload | Excessive notifications and messages within the EHR can overwhelm providers. | Customize alert settings within the EHR to highlight and prioritize critical information, reducing the risk of information overload. Training for staff on effective inbox management and prioritization techniques is also crucial. |
| Patient Portal Access Disparities | Digital literacy barriers and technology access gaps can limit patient portal use, especially among older adults or disadvantaged populations. | To mitigate access disparities, offer tutorials on using the patient portal, which can be delivered in person or via phone. Provide educational materials in multiple languages and formats that are easy to understand. Explore options for assisted access, such as allowing family members designated access to the portal. |
| Interoperability Gaps | Seamless data exchange between different EHR systems remains an evolving area. | Encourage the adoption of interoperability standards across the industry, such as FHIR, to facilitate better data exchange. Engage in regional Health Information Exchanges (HIEs) to enhance connectivity. Choose EHR systems with robust interoperability features. |
When thoughtfully implemented, EHRs show immense potential to improve communication efficiency across the healthcare ecosystem. But technology alone is not the answer. Optimizing use of EHR communication tools while keeping patient needs at the center enables healthcare teams to fully realize the benefits. Smoother information exchange ultimately leads to more informed decision-making and better-coordinated care for patients. That’s a win-win for all.
The adoption and use of electronic health records (EHRs) have become a pivotal priority for healthcare organizations across the country. However, the road to successful EHR implementation is often bumpy. Industry research indicates that nearly 30% of EHR projects fail to achieve their intended outcomes.
Leadership is emerging as one of the most crucial ingredients that separate EHR success stories from failures. But what defines effective leadership for EHR implementation? How can hospitals and health systems build the right leadership team to steer these complex projects to success?
EHR implementations require a diverse leadership team combining technical expertise, clinical knowledge, and change management skills. As you identify and select members of the EHR leadership team, there are some key considerations:
Assembling a leadership team combining these diverse skills and experience levels sets up your EHR implementation for success.

While every EHR project is unique, some leadership roles and responsibilities are consistently important across implementations:
When these roles have clearly defined, yet interconnected responsibilities, EHR project teams can plan, coordinate, and execute implementations effectively.
EHR implementations can profoundly impact clinical and administrative workflows. Leaders who are physically present and actively engaged during rollout foster smoother transitions. Research highlights the benefits of on-site leadership:
While off-site oversight has some benefits, dedicated on-site leadership before, during, and after go-live drives successful user adoption.
Careful team formation and skillful management are crucial for EHR project success. Consider these strategies:
With purposeful team building and management, healthcare organizations can overcome the fragmentation that often derails EHR projects.
Leadership changes and instability can seriously impede EHR success. But there are strategies to navigate them effectively:
With planning and skill, healthcare organizations can manage leadership challenges, staff transitions, and minimize the disruption to EHR rollouts.
EHR success hinges greatly on the active involvement of hospital executives and boards. Their influence can make or break projects through:
Securing active, vocal C-suite sponsorship and oversight is essential for EHR success. Their influence extends throughout the project's lifespan.
More than skills or experience, leadership behaviors and mindset are crucial determinants of EHR implementation success. Consider instilling these behaviors organization-wide:
With visible behavioral commitment from executives down through frontline managers, organizations can rally around a smooth EHR transition.

EHR adoption is a defining priority for modern healthcare leaders. It takes immense skill, perseverance, and teamwork to shepherd these multifaceted projects to success in the face of many potential pitfalls.
We outlined the key research and strategies around building an effective EHR leadership team, fostering excellence through the project life cycle, and demonstrating behaviors that inspire organization-wide commitment. Take these insights to heart.
Rally your best across IT, clinical operations, administration, and strategy around a shared vision. Lead with courage, conviction, and compassion. And you will undoubtedly join the ranks of EHR success stories!
As the healthcare industry evolves, hospitals and health systems are turning to electronic medical record (EMR) and electronic health record (EHR) systems to streamline operations, improve patient care, and meet regulatory requirements.
With many options available, it can be challenging to choose the best fit. In this guide, we'll explore the history, benefits, features, and top systems used by hospitals.
The transition from paper-based medical records to digital EMR/EHR systems has been gradual, spanning decades. In the 1960s and 1970s, a few hospitals began experimenting with electronic record-keeping. Widespread adoption was slow due to high costs, limited functionality, and resistance to change.
In the 1990s and 2000s, computer technology advances and concerns about medical errors and inefficiencies renewed interest in EMR/EHR systems. The HITECH Act of 2009 provided financial incentives for hospitals and providers to adopt certified EHR technology, accelerating the shift to digital records.
Today, the majority of US hospitals use EMR/EHR systems. According to the Office of the National Coordinator for Health Information Technology, as of 2017, 96% of non-federal acute care hospitals had adopted certified EHR technology, but their sophistication and interoperability varies widely.

Implementing an EMR/EHR system requires a significant investment of time, money, and resources, but the potential benefits are substantial and wide-ranging. Some key advantages include:
1. Improved efficiency and productivity: EMR/EHR systems automate manual tasks like chart retrieval, order entry, and prescription refills, saving staff time, reducing paperwork, and streamlining workflows. One study found that nurses in hospitals with advanced EHR systems spent 19% less time on documentation and 24% more on direct patient care than nurses in hospitals with basic EHR systems.
2. Better quality of care and patient outcomes: EMR/EHR systems provide real-time access to current patient information, including medical history, medications, allergies, and test results. This can prevent errors, avoid duplicated services, and support evidence-based decision making. Studies show that hospitals with advanced EHR systems have lower rates of adverse drug events, hospital-acquired infections, and mortality than those with less advanced systems.
3. Cost savings and ROI: Despite the substantial upfront costs of implementing an EMR/EHR system, many hospitals see a positive return on investment through increased efficiency, reduced errors and redundancy, and improved billing and reimbursement. A RAND Health study found that widespread EMR/EHR adoption could yield $81 billion annually in net benefits, driven by savings from improved safety and efficiency.
4. Easier sharing of patient data: EMR/EHR systems facilitate the secure exchange of patient information between providers, hospitals, and other healthcare organizations. This is important in today's fragmented healthcare system, where patients receive care from multiple providers across different settings. Interoperability standards like HL7 and FHIR enable systems to communicate and share data, supporting care coordination and continuity.
5. Enhanced security and reduced risk: EMR/EHR systems provide robust security to protect patient data from unauthorized access, breaches, and cyber attacks. This includes encryption, access controls, audit trails, and backup and disaster recovery.
By reducing reliance on paper records, EMR/EHR systems minimize the risk of lost, stolen, or damaged charts. However, hospitals must still implement strong security practices and comply with HIPAA regulations to safeguard patient privacy.
Most EMR/EHR systems offer a core set of functionalities to support clinical workflows and patient care. Key capabilities include:
EMR/EHR systems allow clinicians to electronically document patient encounters, assessments, and treatment plans using structured templates and free-text fields, creating a legible, searchable record accessible and shareable by authorized users. Many systems also support voice recognition and natural language processing to streamline documentation.
CPOE modules allow providers to enter medication, test, procedure, and referral orders electronically, reducing errors from illegible handwriting, transcription mistakes, and incomplete information. CPOE often includes clinical decision support tools that alert providers to potential drug interactions, contraindications, or dosing errors.
EMR/EHR systems offer real-time guidance and recommendations to clinicians based on evidence-based guidelines, best practices, and patient-specific data. This may include alerts for overdue screenings or immunizations, alternative treatments suggestions, or risk scores for conditions like sepsis or readmissions. By presenting the right information at the right time, clinical decision support can improve quality of care and patient outcomes.
EMR/EHR systems must exchange data with other systems and organizations to support care coordination and population health management. This includes lab and imaging systems, pharmacies, public health registries, and other providers' EHRs. Standards like HL7 and FHIR provide a common language and format for data exchange, while health information exchanges (HIEs) act as hubs for sharing data across communities or regions.
EMR/EHR systems include patient-facing portals for health information access, provider communication, prescription refills, and online appointment scheduling. Some systems offer mobile apps, telehealth capabilities, and remote monitoring tools to support patient engagement. Empowering patients to take an active role in their care can improve satisfaction, adherence, and outcomes.
Hospitals use various Electronic Medical Record (EMR) systems to manage patient information and healthcare operations. The most common EMR systems include those provided by Epic Systems Corporation, Oracle Cerner, and MEDITECH, among others. These systems are designed for inpatient settings and are chosen for their comprehensive functionality and integration with other healthcare services and departments.
The most used EMR system in hospitals is provided by Epic Systems Corporation, holding nearly 38% of hospital installations in the United States. Oracle Cerner follows with about 22% of the U.S. hospital EHR market share. These systems are preferred for usability, advanced features, and integration with healthcare services.
Most hospitals use EMR systems to support inpatient care. The most commonly used systems are developed by Epic Systems Corporation and Oracle Cerner, due to their comprehensive features and widespread adoption in the healthcare industry.
The provided web pages do not list four specific types of EMR, but EMR systems can be categorized based on their functionality and healthcare settings. These include certified EMR systems, cloud-based EMR systems, mental health EMR systems, and EMR systems for specific medical specialties or practice sizes.
An example of an EMR is the system provided by Epic Systems Corporation, widely used across healthcare settings, including community hospitals, academic medical centers, and independent practices. Epic's EMR system is known for its robust features and ability to integrate with other healthcare services.
With so many EMR/EHR options available, hospitals must carefully evaluate their needs and priorities when selecting a system. Some key factors to consider include:
1. Size and type: Larger hospitals and integrated delivery networks may need enterprise-level solutions, while smaller hospitals and critical access facilities may prioritize ease of use and affordability. Specialty hospitals may need EHRs with specific modules, such as oncology or behavioral health.
2. Integration with existing systems: Hospitals have complex IT systems like lab, radiology, and pharmacy. It's important to choose an EHR that can seamlessly integrate with these systems to avoid data silos and workflow disruptions.
3. Interoperability and data sharing: As value-based care and population health initiatives gain traction, hospitals need EHRs that can easily share data with other providers, payers, and public health entities. Look for systems that support standards like HL7 and FHIR, and participate in health information exchanges.
4. Vendor experience and market share: Consider the vendor's track record in the hospital EHR market, including experience with similar-sized organizations and overall market share. A larger market share may indicate a more stable and well-resourced vendor, but potentially less personalized service.
5. Total cost of ownership: Besides initial software and hardware costs, hospitals must consider ongoing expenses like maintenance, upgrades, training, and support. Some vendors offer subscription-based or pay-as-you-go pricing models that are more affordable for smaller hospitals.
6. Cybersecurity and compliance: Hospitals must prioritize EHR security and compliance with regulations like HIPAA due to the increasing threat of cyber attacks and data breaches. Look for vendors with strong security features, such as encryption, access controls, and monitoring, and a track record of protecting patient data.
7. User experience and training: An EHR is only as effective as its users, so choose a system with an intuitive, user-friendly interface and robust training and support resources. Consider the vendor's approach to implementation and training, as well as their ongoing customer support and user community.
Choosing an EMR system involves considering factors like practice size, medical discipline, and needed features. Look for a system that improves workflows, offers interoperability, and has a patient portal. The system should support clinical decision-making and reduce errors. Review top EMR systems used by peers and consider cost, usability, and vendor support.
Despite significant EMR/EHR progress, hospitals still face challenges in optimizing these systems for quality, safety, and efficiency. Some key issues include:
1. Usability and physician burnout: Many clinicians report that EHRs are time-consuming, cumbersome, and distracting, contributing to burnout and dissatisfaction. Hospitals must work with vendors to streamline workflows, reduce click fatigue, and tailor systems to specific specialties and user roles.
2. Interoperability and data blocking: Despite improved standards, many hospitals still struggle to exchange data effectively with other systems and organizations. Vendors may engage in data blocking, restricting the flow of information, and legacy systems may lack necessary interfaces and protocols.
3. Cybersecurity and privacy: As EHRs become more interconnected and cloud-based, they're more vulnerable to cyber attacks and data breaches. Hospitals must invest in robust security measures, such as encryption, access controls, and monitoring, and train staff on best practices for protecting patient data.
4. Cost and maintenance: Implementing and maintaining an EHR system can be a financial burden for hospitals, especially smaller and rural facilities. They must balance advanced functionality with limited budgets and IT resources.
The future of EMR/EHR systems will be shaped by key trends and innovations, including:
1. Artificial intelligence and machine learning: AI and ML technologies can transform EHRs by automating tasks, identifying patterns and anomalies, and providing personalized clinical decision support. For example, AI algorithms could analyze patient data to predict readmission risk, suggest treatment plans, or flag errors or omissions in documentation.
2. Voice recognition technology improvements may lead to EHRs incorporating virtual assistants and natural language processing to streamline documentation and information retrieval. Clinicians could dictate notes, order tests, and retrieve patient data using conversational interfaces, reducing the need for typing and clicking.
3. Blockchain and distributed ledgers: Blockchain technology could enable secure, decentralized sharing of patient data across organizations and systems. By creating an immutable, tamper-proof record of transactions and permissions, blockchain could help overcome trust and interoperability challenges in current EHR systems.
4. Patient-generated health data: As wearables, remote monitoring devices, and mobile health apps become more common, EHRs will need to incorporate more PGHD for a comprehensive view of patient health and behaviors. This could enable proactive, personalized care and support population health management.
5. Social determinants of health: There is growing recognition that social and environmental factors, like housing, education, and access to healthy food, play a significant role in health outcomes. Future EHRs may include more data on social determinants of health (SDOH) to help clinicians identify and address barriers to health and well-being.

EMR/EHR systems are essential for hospitals and health systems to improve patient care quality, safety, and efficiency. By digitizing and integrating patient data, these systems support clinical decision making, care coordination, and population health management.
However, choosing and implementing the right EMR/EHR system requires careful consideration of an organization's specific needs, priorities, and resources.
As healthcare evolves, EMR/EHR systems must adapt to meet the changing needs of patients, providers, and payers. This may involve incorporating new technologies like AI and blockchain, integrating patient-generated and social determinants data, and prioritizing interoperability and data sharing.
Hospitals that effectively use EMR/EHR systems to drive quality improvement, cost savings, and patient engagement will thrive in the value-based care era.